Arthritis is one of humanity’s leading cause of disability. The commonest type of arthritis experienced in knees, hips and shoulders is osteoarthritis, which is associated with wear or breakdown of the cartilage. This can cause pain, swelling, stiffness and deformity.

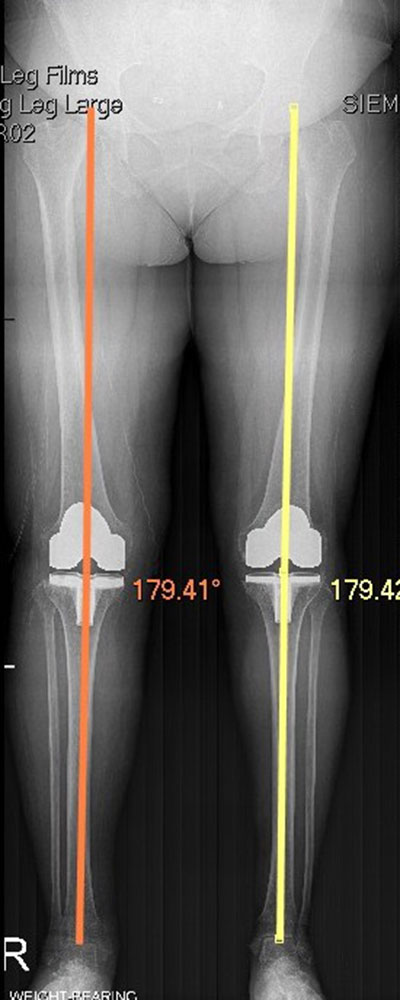
X-ray showing advanced osteoarthritis of both knees.
Dr Sunil Reddy specialises in Total Joint replacement surgery of Knee, hip and shoulder. He strives to achieve the best possible outcomes and improve the quality of life of his patients. Towards the same objective, he utilises computer navigation in all Total knee replacement surgeries and also offers Robotic-assisted Total knee replacements. He also utilises Patient-specific technology in shoulder replacement surgery.


Bone model and X-ray image of a Total knee replacement prosthesis.
Total Knee Replacement (TKR) or Total knee arthroplasty is one of the most successful treatments in medicine. It provides effective relief in pain and improvement in function in the vast majority of patients undergoing the procedure. It allows patients to return to activities and hobbies they loved to do.
TKR may be required for patients suffering from a range of conditions affecting the knees, including:
- Severe osteoarthritis is the commonest indication.
- Rheumatoid arthritis.
- Arthritis secondary to severe gout, pseudogout and bleeding disorders are less common indications for a knee replacement.
- Osteonecrosis (also known as avascular necrosis) - death of bone tissue caused by lack of blood supply.
Procedure
The procedure involves the replacement of the knee joint with a prosthesis, that is an artificial joint.
The procedure generally takes about 90 minutes to complete and is performed under a general anaesthetic or a spinal/epidural anaesthetic. Femoral nerve block is often used as a part of multi-modal peri-operative pain management.
Dr Sunil Reddy has special interest in pain management and bleeding control following TKR. He routinely uses LIA (Local infiltrative anaesthesia) and tranexamic acid to minimise bleeding from surgery.
The surgery is performed through an incision in front of the knee joint. Following exposure of the joint, careful and accurate cuts of the distal femur (thigh bone) and proximal tibia (shin bone) are performed to seat the prosthetic components.
The goals of a knee replacement surgery are restoration of limb alignment, appropriate ligament balance and a well tracking extensor mechanism (patella and its tendon attachments).
New technologies are increasingly being used to achieve these goals. Computer assisted surgery (CAS) in Total knee arthroplasty, abbreviated to CAS-TKA and Robotic-Assisted TKA are some of such technologies.
Learn more about Total Knee Replacement, including:
- Computer navigation in Total Knee Replacement
- Robotic-Assisted Total Knee Replacement
- Patient-specific technology in Total Knee Replacement


Computer navigation allows for reliable and reproducible restoration of limb alignment in total knee replacements. It helps achieve precision and accuracy especially in patients with a large body habitus and in post-traumatic bone deformities (two images at bottom).
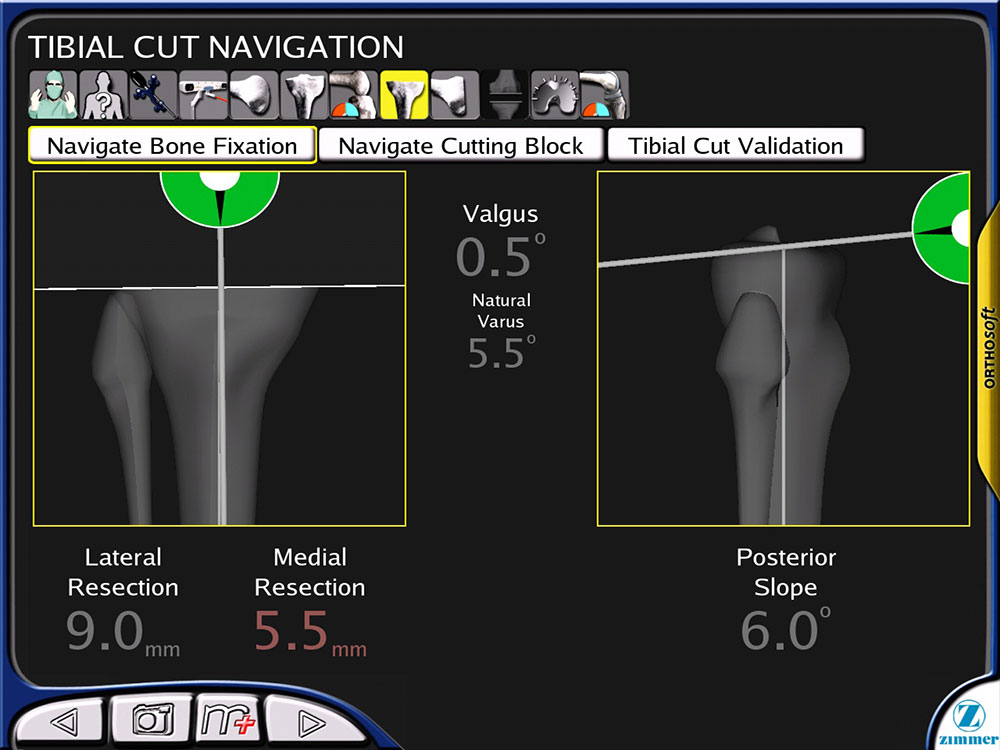
Screen-shot of bone cuts being performed during CAS-TKA.
An intuitive new device in the CAS group of devices has been introduced recently – iAssist device - which uses small electronic pods which are essentially small computers with wireless technology (like our smartphones). The device which fits onto TKR instrumentation registers the anatomic axis specific to that patient and enables us to restore the mechanical axis precisely and reproducibly.
Robotic-Assisted Total Knee Replacement
Robotic technology was harnessed to improve alignment and position of knee replacement prosthesis – both total and partial knee replacements – more recently. Long-term results are not available for this technology in published medical literature at this stage and it is not yet known if it is going to make a significant difference in functional outcomes. Based on short term studies, it seems to hold a lot of promise and evolving to position itself as the Joint Replacement technology of the future. Sunil Reddy offers Robotic-assisted Total knee replacements to all his patients. As a part of the Joint Replecement Clinic (JRC) he offers this technology at No-out-of-pocket expense to all privately insured patients.
Please download the information sheet below for factual information and thoughts on Robotic-assisted TKR compiled by Dr Sunil Reddy.
Download Robotic-Assisted Total Knee Replacement – an evidence based guide for patients (PDF).
Patient-specific technology in Total Knee Replacement
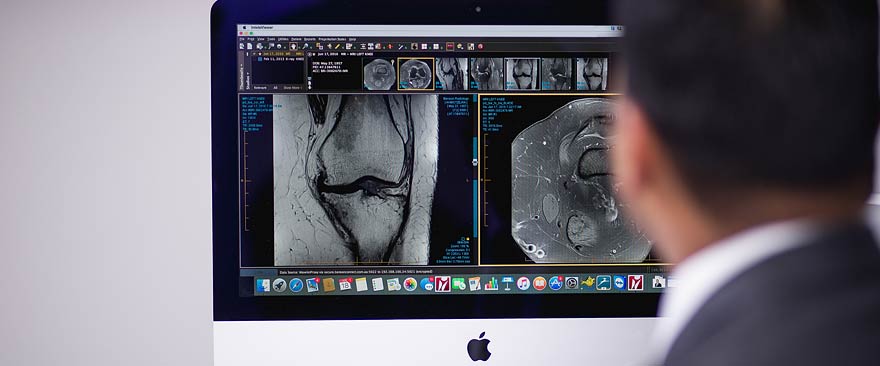
Patient-specific Instrumentation (PSI) in Joint replacement is an MRI based 3D-prototyping technology where 3D models of the arthritic joint as well as jigs specific to the patient’s anatomy are manufactured. These are then used during surgery to make accurate bone cuts and implant the prosthesis.
PSI is an evolving technology. Limited available literature does not clearly support significant improvement of postoperative pain, activity, function, or ROM when PSI is compared with conventional TKR instrumentation. But it has its advantages in some patients where use of intramedullary guides is not possible or desirable and patients with post-traumatic limb deformities. PSI also enables the surgeon to preoperatively better appreciate bone defects in advanced osteoarthritis and preoperatively plan bone cuts, implant position, implant size, and need for augments.
PSI has a useful role in accurate positioning of glenoid (socket) component in Shoulder replacement. This is discussed under Total Shoulder Replacement and Reverse Total Shoulder Replacement.
You and your TKR – Things you need to know
Overview of benefits
Total hip and knee replacement surgeries are incredibly advanced and time-tested treatments that significantly improve your quality of life and let you pursue activities and hobbies you loved to do. 9 out of 10 patients are generally happy with the results of total knee replacement surgery, with most of the previous pain disappearing.
Overview of risks
Injury to blood vessels and nerves (rare complication), Infection (less than 1 in 100 surgeries on an average), blood clots in the leg veins or lungs (Deep venous thrombosis, Pulmonary embolism), stiffness of the knee following surgery and anaesthetic complications are some of the risks of this major surgical procedure.
Although the artificial joint may well last a lifetime, it may also wear out over time, or may come loose, in which case a revision knee replacement surgery may be required.
In symptomatic advanced knee arthritis, the benefits of the procedure far outweigh the risks associated. Dr Sunil Reddy will discuss with you the benefits, risks and complications at the time of initial consultation and help you make the best choice of treatment.
Hospital stay
Most patients go home within three days after a knee replacement. This is in part made possible by an evidence based multi-modality pain relief protocol as well as blood loss minimisation measures that Dr Reddy ensures for all his arthroplasty patients.
Some patients need an overnight observation in HDU (High dependency unit) or ICU (Intensive care unit).
Dr Reddy and the physiotherapist will see you on the same evening or next day morning and get you up and about and doing exercises/walking as you can tolerate.
You can go home when you can walk around and feel confident and comfortable to take care of yourself at home, often with some assistance from your family or friend.
Pain Relief and Blood-loss minimisation
Pain relief during and after your surgery is a priority to my team. Our anaesthetists are experienced in multi-modality pain relief which includes nerve blocks, IV and oral analgesics and LIA (Local infiltrative analgesia performed by me as a part of the surgery). Appropriate anaesthesia and IV tranexamic acid in the peri-operative period aid in minimising blood loss and ensure a very low blood transfusion requirement. Identifying and appropriate treatment of anaemia and iron deficiency prior to surgery is an important part of the pre-operative evaluation of TKR. If your blood haemoglobin is low, Dr Reddy may advise a period of iron therapy before surgery to give you the best chance of an optimum recovery following surgery.
Wound Care
Dr Reddy will see you in the Clinic between 12 to 14 days after surgery. The sutures are absorbable ones that do not need removal. Please keep the wound clean and dry. The dressing is waterproof enabling you to take a shower.
Please do not remove the dressing before the clinic visit to minimise the risk of infection.
Please do not start antibiotic therapy for perceived wound problems without conmsulting Dr Reddy
Call Dr Reddy’s Rooms if you have any concerns with excessive pain, redness or discharge from the wound site or feel unwell.
Follow-up with Dr Reddy would be organised at 2 weeks, 6 weeks, 3 months, 1 year and 5 years following your surgery.
Rehabilitation Guidelines following Total Knee Replacement
- The time-lines mentioned are approximate and actual progression depends on individual recovery.
- Patients can weight bear as tolerated from day 1. Please use a walker or crutches till good pain control, quadriceps strength and walking mechanics are achieved.
- Avoid pillow under knees and focus on knee extension and quadriceps exercises from day 1. Limb elevation with pillow under ankles/calves when lying is recommended.
- Apply Ice packs 3-5 times for 10 min each time for the first two weeks.
First 2 weeks
Quadriceps and gluteal sets, proprioception and balance exercises (e.g. Heel-to-toe walking).
- Straight leg raises.
- Active and passive Range of Movement exercises.
- Gait training.
- Upper body conditioning.
- Please remember to apply Ice packs 5 times daily for 10 min; take pain medication as advised and follow the advice of your therapist.
2 to 6 weeks
- Continue with the Home exercise program.
- Progress to walking outside.
- Progress with Quadriceps, ROM and proprioception/balance exercises.
- Start Core strengthening exercises.
- Hydrotherapy / Pool work-outs once incisions have healed.
- Aerobic exercises after 4 weeks as tolerated (e.g. Static exercise bike).
6 to 12 weeks
- Add lateral steps and step-ups.
- Single leg stance (eccentric exercises initially).
- Progress with all functional activities including household chores, gardening, gentle sporting activities.
- Low impact activities only till 3 months.
- No twisting, pivoting till 3 months.
- Wean into a home/gym program.
References
- Mason JB, Fehring TK, Estok R, Banel D and Fahrbach K. (2007) Meta-analysis of alignment outcomes in computer-assisted total knee arthroplasty surgery. J Arthroplasty. 22(8):1097–1106.
- Fickert S, Jawhar A, Sunil P, Scharf HP. Precision of Ci-navigated extension and flexion gap balancing in total knee arthroplasty and analysis of potential predictive variables. Arch Orthop Trauma Surg. 2012 Apr;132(4):565-74. doi: 10.1007/s00402-011-1419-x. Epub 2011 Nov 11.
- Nick Pourgiezis, Sunil P Reddy, Mark Nankivell, Gordon Morrison, John VanEssen, Alignment and component position after patient-matched instrumentation versus conventional total knee arthroplasty. Journal of Orthopaedic Surgery 2016;24(2):170-4.
Related Topics
Rehabilitation Guidelines following Total Knee Replacement